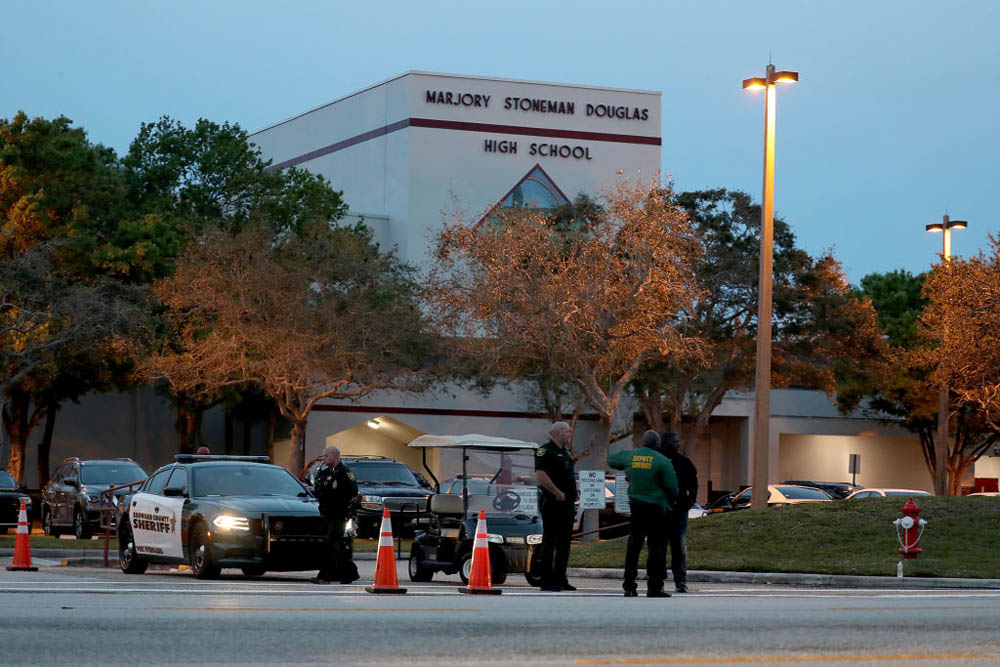
Nikolas Cruz, the 19-year-old whose alleged shooting rampage claimed 17 lives at Marjory Stoneman Douglas HS, in Parkland, Fla., was sick. His family knew it. His neighbors knew it. Local law enforcement and mental-health professionals knew it. Yet, like so many tragedies involving the seriously mentally ill, no one was able to prevent the rampage. Why?
As someone with a family member with serious mental illness, and has spent 30 years helping other families with seriously ill members, the answer is clear: The system often prevents relatives from getting help for loved ones who have serious mental illness until after they have become a danger to themselves or others. Too often this means after someone — often a family member — is injured or killed.
An NPR investigative report found Cruz was “the subject of dozens of 911 calls and at least two separate tips to the FBI.” Most were for threats or acts of violence against his family, including apparently holding a gun to his mother’s and brother’s heads. His father died in 2004 and his mother died last November, leaving him with little family support.
Family are often the caretakers and, as a result, too often victims of violence. In a 2016 report by the nonprofit Treatment Advocacy Center, my co-authors and I found that serious mental illness (typically untreated) is associated with an estimated 29 percent of family homicides and 7 percent of all homicides. In 2013, these fatalities outstripped deaths related to meningitis, kidney infection or Hodgkin’s disease.
Yet too often, mental-health advocates hide behind the platitude that the mentally ill are no more violent than others. That may be true for those being properly treated, but not for the untreated, including those suffering from schizophrenia or bipolar disorder.
We families with seriously ill members know that — and hope lawmakers now listen to us, rather than to the mental-health industry.
A major problem is that the federal government doles out around $150 billion in mental-health funding, but doesn’t require programs to serve the seriously mentally ill. Instead, the funds often go to improve “wellness” in the general population through yoga classes or “mindfulness” training.
We can help stop future Parklands by focusing our spending on those who need help the most and are most likely to become dangerous without that help. Here are six suggestions that would save lives and help families get loved ones the treatment they need:
- Increase the number of available psychiatric beds by eliminating a Medicaid rule that forbids states from using Medicaid funds for seriously mentally ill adults who need long-term hospitalization.
- End the practice of requiring someone to become dangerous before their families can intervene to help them. We could do that by supplementing the standard by which we commit mentally ill people to health facilities — presently “danger to self or others” — to also include “need for treatment,” “grave disability” and “lack of capacity.”
- Pass strong assisted-outpatient-treatment laws so judges can order the most seriously mentally ill to stay in treatment. A 2017 Manhattan Institute report found that New York state assisted-outpatient treatment reduced rates of arrests by 83 percent and incarceration by 87 percent. It also led to a 77 percent fall in hospitalization and a 74 percent drop in homelessness.
- Free parents of mentally ill children from the handcuffs of health-privacy laws so they can learn what is wrong with their kids, as well as help refill prescriptions and facilitate treatment compliance.
- Allow people to take out restraining orders (“red-flag orders”) to remove guns from mentally ill people who threaten themselves or others, and prevent them from making firearms-related purchases.
- Finally, rein in the Protection and Advocacy for Individuals with Mental Illness program and the Justice Department’s Civil Rights of Institutionalized Persons Act division. PAIMI defends the right of the psychotic to refuse treatment, while CRIPA has brought lawsuits against state hospitals, resulting in people with serious mental illness moving into community settings. Eliminating those activities would make it easier for families to facilitate appropriate care for our loved ones.
Denial of the association between serious mental illness and violence may be politically correct and well-intended. But, too often, it ends in tragedies such as the Parkland shooting — and another scramble for answers we already have.
This piece originally appeared at the New York Post
______________________
DJ Jaffe is Executive Director of Mental Illness Policy Org., and author of Insane Consequences: How the Mental Health Industry Fails the Mentally Ill.
This piece originally appeared in New York Post